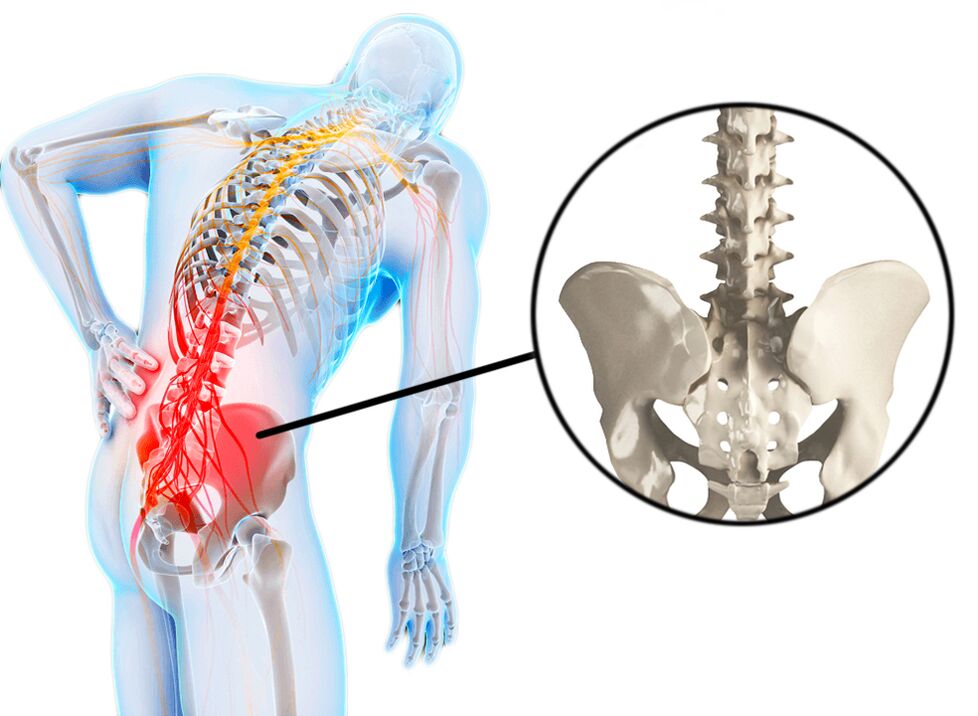
Low back pain is often referred to as lumbago or lumbodynia. Lumbago, or "lumbago, " is an attack of acute low back pain, usually associated with hypothermia and tension. Lumbago occurs in many people and is often the cause of temporary disability. Often, sports injuries or sprains can be the cause of lumbago, but sometimes the factor that triggers the appearance of pain remains unknown. Lumbago is characterized by pain that does not spread to the legs. Low back pain (lumbago) may be acute and may progress gradually throughout the day. Often there is stiffness in the morning, and gradually the stiffness turns into a pain syndrome. Spinal curvature (antalgic scoliosis) as a result of muscle spasm is also possible. The pain itself may be associated with muscle spasms, which in turn are associated with other causes. These can include overuse or sprains, sports injuries, herniated discs, spondyloarthritis (spondylosis), and kidney disease (infections or kidney stones). Sometimes the patient clearly identifies the cause-and-effect relationship between tension, hypothermia, and the appearance of the disorder, but often the pain appears for no apparent reason. Sometimes back pain can even occur after sneezing, bending over, or wearing shoes. This can be facilitated by deforming diseases of the spine, such as scoliosis.
Unlike lumbago, the term lumbodynia does not mean acute pain, but semi-acute or chronic pain. As a rule, the pain with lumbodynia appears gradually over several days. Pain can also occur in the morning and may be reduced by physical activity. Lumbodynia is characterized by increased pain during prolonged static loads (sitting, restless body position). Lumbodynia is also characterized by prolonged pain relief. Patients with lumbodynia have difficulty performing daily activities such as washing or wearing shoes due to muscle spasms. Due to the disease, the volume of body movements decreases (forward bending or to a lesser extent to the side or stretching). Because of the pain syndrome, the patient often has to change position when he needs to sit or stand. Unlike lumbago, muscle spasm is less pronounced and, as a rule, does not cover the entire lower back, and often there are signs of the spread of spasm on one side.
Causes of back pain
Back pain is a symptom. The most common causes of back pain are diseases (injuries) of muscles, bones and intervertebral discs. Sometimesback, back paincan cause diseases of the abdomen, small pelvis and chest. Such pains are called reverse pains. Diseases of the abdominal cavity (eg, appendicitis), aortic aneurysm, kidney disease (urolithiasis, kidney infection, bladder infections), infections of the pelvic organs, ovaries - all these diseases can manifest themselves.back, back pain. . . Even a normal pregnancy can cause pelvic floor twitching, muscle spasms due to stress, and back pain due to nerve irritation.
Oftenback, back painassociated with the following diseases:
- Compression of the nerve root, which causes sciatica symptoms and is most often caused by a herniated disc. As a rule, when the nerve root is compressed, the pain becomes sharp, radiation and sensitivity in the innervation zone of the nerve root is impaired. Disc herniation occurs primarily as a result of disc degeneration. There is swelling of the gelatinous part of the disc from the central cavity and pressure on the nerve roots. Degenerative processes in the intervertebral discs begin at the age of 30 and older. However, the presence of hernias does not always affect the nerve structures.
- Spondylosis - degenerative changes in the vertebrae themselves, bone growths (osteophytes), which can affect nearby nerves, causing pain.
- Spinal stenosis can occur as a result of degenerative changes in the spine (spondylosis and osteochondrosis). A patient with spinal stenosis in the lumbar region may experience back pain that spreads to both legs. Low back pain can appear as a result of standing or walking.
- Cauda equina syndrome. This is an ambulance. Cauda equina syndrome occurs as a result of compression of the elements of the cauda equina (terminal part of the spinal cord). A patient with Cauda equina syndrome may experience pain, bowel and bladder dysfunction (urinary incontinence and atony). This syndrome requires emergency surgery.
- Pain syndromes such as myofascial pain syndrome or fibromyalgia. Myofascial pain syndrome is characterized by pain and soreness at certain points (trigger points), a decrease in the volume of muscle movement in the painful areas. Pain syndrome is reduced by relaxing the muscles located in the painful areas. Pain and soreness with fibromyalgia are common throughout the body. Fibromyalgia is not characterized by compression and muscle pain.
- Bone infections of the spine (osteomyelitis) are rarely the cause of the disease.
- Non-infectious inflammatory diseases of the spine (ankylosing spondylitis) can cause stiffness and pain in the spine (including in the lower back), which worsens, especially in the morning.
- Tumors, most cancerous metastases, can be a source of back discomfort.
- Inflammation of the nerves and therefore the manifestations of pain (in the chest or lumbar region) can damage the nerves themselves (for example, with shingles)
- Given the different causes of symptoms, such as acute or subacute back pain, it is important to fully assess the patient and perform all necessary diagnostic procedures.
Symptoms
Pain in the lumbar-sacral region is the main symptom of lumbago, lumbodynia, lumboishalgia.
- The pain may spread to the front, side, or back of the foot (lumbar spine) or may be localized only in the lumbar region (lumbago, lumbodynia).
- Pain in the lower back may increase after tension.
- Sometimes the pain can be exacerbated at night or when sitting for long periods of time, such as during a long car trip.
- Perhaps numbness and weakness in the part of the foot located in the area of innervation of the compressed nerve.
Special attention should be paid to a number of criteria (symptoms) for timely diagnosis and treatment:
- Recent injury history, such as a fall from a height, a traffic accident, or similar events.
- Presence of minor injuries in patients over 50 years of age (eg, slipping and falling over the hip).
- History of long-term use of steroids (for example, these are patients with bronchial asthma or rheumatic diseases).
- Any patient with osteoporosis (mostly older women).
- Any patient over the age of 70: at this age there is a high risk of cancer, infection and diseases of the abdominal organs, which can lead to back pain.
- History of oncology
- Presence of infectious diseases in the recent past
- Temperature above 100F (37, 7 C)
- Drug use: Drug use increases the risk of infectious diseases.
- Low back pain worsens at rest: as a rule, this nature of the pain is associated with oncology or infections, and such pain can also be associated with ankylosing spondylitis (ankylosing spondylitis).
- Significant weight loss (without any obvious reason).
- The presence of any acute nerve dysfunction is a signal for emergency medical care. For example, these are gait disturbances, leg dysfunction, and, as a rule, signs of acute nerve damage or compression. Under certain conditions, such symptoms may require urgent neurosurgery.
- Bowel or bladder dysfunction (both abduction and urinary retention) may be a sign of emergency medical care.
- Failure of recommended treatment or increased pain may also require medical attention.
The presence of any of the above factors (symptoms) is a signal to seek medical attention within 24 hours.
Diagnostics
A medical history is important to make an accurate diagnosis, as various conditions can cause back pain. Time of onset of pain, contact with physical force, cough, fever, bladder or bowel dysfunction, convulsions, etc. Physical examination is performed: identification of pain points, the presence of muscle spasms, the study of the neurological condition. If there is a suspicion of diseases of the abdominal cavity or pelvic organs, an examination is performed (ultrasound of the abdominal organs, ultrasound of the pelvis and pelvic organs, urine blood tests).
If the somatic genesis of low back pain is ruled out, instrumental research methods such as radiography, CT, or MRI may be indicated.
X-ray is a method of initial examination and allows to determine the presence of changes in bone tissue and indirect signs of changes in the intervertebral discs.
CT allows you to visualize the presence of various changes in both bone tissue and soft stones (especially in contrast).
MRI is the most informative research method that allows to diagnose morphological changes in various tissues.
Densitometry is required when osteoporosis is suspected (usually in women over 50).
EMG (ENMG) is used to detect conduction disturbances along nerve fibers.
Laboratory tests (blood tests, urine tests, blood biochemistry) are usually prescribed to rule out inflammatory processes in the body.
Pain treatment
After diagnosis and confirmation of vertebral genesis with lumbago and lumbodynia, a specific treatment is prescribed for low back pain.
In acute pain need 1-2 days of rest. Bed rest can reduce muscle tension and muscle spasms. In most cases, when the pain syndrome is associated with muscle spasms, the pain syndrome subsides for a few days without medication, just for rest.
Medication. NSAIDs are used for pain syndrome. The side effects of COX-2 inhibitors are less, but long-term use of these drugs also carries certain risks. Given that all drugs in this group have many side effects, the use of drugs in this group should be short-term and under the mandatory supervision of a physician.
Muscle relaxants can be used to relieve spasms. However, the use of these drugs is effective only when there is a spasm.
Steroids can be used to treat pain, especially when there are symptoms of sciatica. However, due to the obvious side effects, the use of steroids should be selective and short-term.
Manual therapy. This technique can be very effective when there is subluxation of muscle blocks or facet joints. Mobilization of motor segments can reduce both muscle spasm and back pain.
Physiotherapy. There are many modern physiotherapy procedures (eg, electrophoresis, cryotherapy, laser therapy, etc. ) that can reduce both pain and inflammation and improve microcirculation.
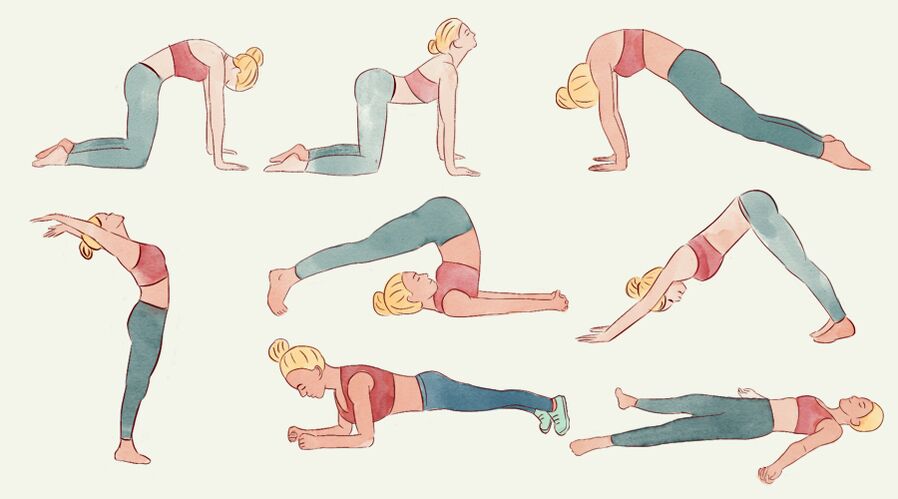
Exercise therapy. Exercise is not recommended for acute back pain. The connection to exercise therapy is possible after reducing the pain syndrome. In the case of chronic pain, exercise can be very effective in strengthening the muscle corset and improving the biomechanics of the spine. Exercise should only be chosen by an exercise therapy physician, as often independent exercise can lead to an increase in pain manifestations. Systemic exercise therapy can maintain spinal function and significantly reduce the risk of pain syndrome, especially in the presence of degenerative changes in the spine (osteochondrosis, spondylosis).

















































